מחלת פיירוני (Peyronie’s disease) מערבת הצטלקות של מעטפת רקמת הפין, הגורמת לעקמת של האיבר ולהפרעות זקפה. מהם הגורמים למחלה וכיצד מטפלים בה? כל ההסברים במאמר שלפניכם.
היה זה דוקטור דה לה פיירוני, רופאו של המלך לואי ה-15, שתיאר לראשונה לפני 250 שנה את המחלה הנקראת על שמו ואת דרכי הטיפול בה. מדובר במחלה המתבטאת בעקמת של הפין, המתפתחת במהלך החיים (בניגוד לעקמת פין מולדת המתפתחת בתקופת העוברות) ומשנה את מבנה הפין באופן שעלול להפריע לתפקוד מיני תקין. זה קורה כאשר נוצרת רקמת צלקת נוקשה המכונה פלאק במקומות שונים בטוניקה אלבוגינאה – המעטפת של גופי הזקפה, אשר מחליפה את הרקמה האלסטית שמאפשרת לפין להזדקף, להתארך ולהתקשות בעת זקפה. בפועל, רקמת הצלקת מושכת כלפיה את הרקמה העדינה המקיפה אותה ובכך גורמת לפין להתעקם בזמן זקפה.
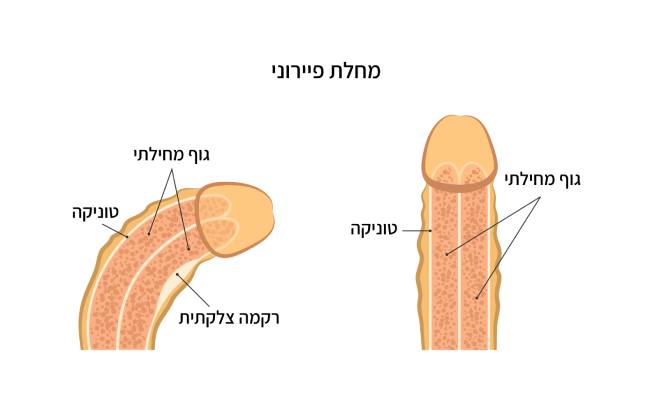 איור 1: חתך של הפין המראה עקמת בזמן זקפה, עקב שקיעת פלאק והיווצרות רקמת צלקת
איור 1: חתך של הפין המראה עקמת בזמן זקפה, עקב שקיעת פלאק והיווצרות רקמת צלקת
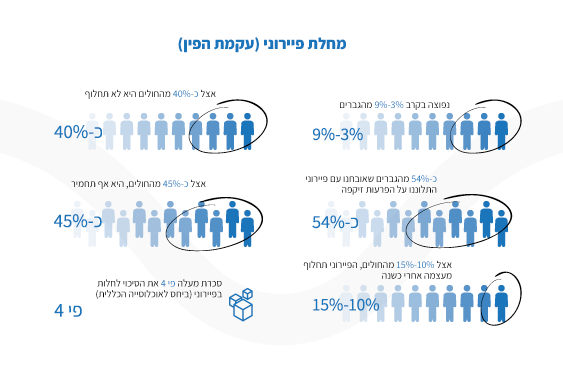
מחלת פיירוני מופיעה בכ-3-9% מהגברים, לרוב בגילאי 40 ומעלה. למרות ששכיחותה עולה עם הגיל היא יכולה להופיע גם בנערים מתבגרים, כאשר מידת החומרה שלה משתנה מגבר לגבר.
הסימפטומים של מחלת פיירוני
הסימפטום המרכזי של מחלת פיירוני הוא היווצרות רקמת צלקת שטוחה (פלאק) בטוניקה אלבוגינאה, שניתן לחוש בה במישוש של העור. עם הזמן הנגעים עוברים תהליך של הסתיידות והופכים לקשים. לרוב ההצטלקות נוצרת בחלק העליון של גוף הפין וגורמת לו להתעקל כלפי מעלה, למרות שהיא עשויה להיווצר גם בצדדים או בחלק התחתון של הפין ולגרום לו להתעקם הצידה או כלפי מטה, בהתאמה. יש גם מצבים בהם רקמת הצלקת מתהווה באופן מפושט על פני כל גוף הפין וגורמת להיצרות שלו ולעיוות בצורת שעון חול המכונה “צוואר בקבוק” (Bottle-neck).
סימפטומים נוספים שעשויים לגרום להפרעות זקפה ובעיות בתפקוד המיני כוללים: ירידה בנוקשות הזקפה, כאבים בזקפה ובעת יחסי המין, כיווץ או התקצרות של הפין בעת זקפה ולפעמים גם במצב רפוי. במחקר שפורסם בכתב העת ‘אורולוגיה’ (Urology) צוין כי יותר מ- 54% מהגברים המאובחנים עם מחלת פיירוני מדווחים על הפרעות זקפה אולם לא בכל המקרים המחלה מפריעה לקיום יחסי מין.
למחלת פיירוני יש גם השפעות פסיכולוגיות ומחקרים מראים כי גברים רבים הלוקים במחלה מתמודדים עם רמה מסוימת של מתח, חששות ודאגות בכל הקשור ליכולת לקיים יחסי מין מספקים ואף בהקשר של הנראות הפיזית שלהם. רבים חווים חרדה לפני או במהלך האקט המיני, ירידה בביטחון העצמי ולעיתים גם דיכאון וירידה באיכות החיים הכללית.
השלב האקוטי והשלב הכרוני
למחלת פיירוני יש שני שלבים כאשר כל של מתאפיין בסימפטומים שונים:
- השלב האקוטי – מכונה גם השלב המוקדם או הדלקתי. בשלב זה נוצרים נגעי פלאק על המעטפת של הפין כחלק מתהליך של דלקת חריפה. הגבר חווה חוסר נוחות או בכאב בעת זקפה והפין מתחיל להתעקם. כשמתחילה להיווצר רקמת צלקת הזקפה עשויה להכאיב. שלב זה נמשך עד כ- 18 חודשים, כשאצל מרבית החולים הכאב יחלוף מעצמו תוך 7-5 חודשים.
- השלב הכרוני – זהו השלב שלאחר יצירת הפלאק שלרוב מתרחש בין 12-18 חודשים מתחילת הסימפטומים הראשוניים. במהלכו נבלם תהליך יצירת הפלאק והעקמת מתייצבת ולא מחמירה. הכאב או אי-הנוחות בדרך כלל פוחתים בעת זקפה אולם יש גברים שממשיכים לחוות הפרעות בזקפה או אפילו החמרה בהן.
חשוב לזכור כי הביטוי של המחלה ומהלכה משתנים מחולה לחולה ומחקרים מצאו כי בכ-15%-10 מהחולים המחלה תחלוף מעצמה בתוך שנה מהאבחון, בכ-40% תישאר ללא שינוי ובכ-45% היא תחמיר.
מדוע זה קורה? על הגורמים למחלת פיירוני
הסיבות להתפתחות מחלת פיירוני עדיין אינן מובנות במלואן, אולם על פי הסברה הרווחת היא נוצרת על רקע חבלה שלרוב (אך לא בהכרח) נגרמת מכיפוף של איבר המין בזמן חדירה בעת קיום יחסי מין או בעת אוננות. חבלה בנסיבות אחרות כוללת למשל פציעת ספורט או תאונה. כפועל יוצא נוצרים קרעים מיקרוסקופיים ברקמת הטוניקה אלבוגינאה ודימום בין השכבות שלה, מה שגורם לתגובה דלקתית המתבטאת לבסוף ברקמת צלקת. יש מטופלים שאינם מודעים לפציעה העדינה בזמן התרחשותה ורבים כלל אינם זוכרים אירוע ספציפי שהתרחש ממש לפני תחילת הסימפטומים.
מלבד זאת, חלק מהחוקרים טוענים כי יתכן ולמחלת פיירוני יש רקע אוטואימוני, כלומר מערכת החיסון היא זו שתוקפת תאים ברקמת הטוניקה אלבוגניאה וגורמת לתגובה הדלקתית והיווצרות רקמת צלקת.
בספרות הרפואית צוינו מספר גורמי סיכון המקושרים לעלייה בסיכון להתפתחות המחלה כגון:
- מחלות של רקמת חיבור – כמו ‘כוויצת דופויטרן’ (Dupuytren contracture) – מחלה תורשתית המופיעה בכשליש מהחולים במחלת פיירוני, אשר מערבת כיווץ של סיבי הגידים בשרירי כף היד; סקלרודרמה – מחלה הגורמת להתנפחות או כאב בשרירים ובמפרקים עקב התפתחות של נגעים מעובים ברקמת חיבור; דורבן – דלקת ברצועה המתחברת לעצם העקב.
- ניתוח בבלוטת הערמונית על רקע גידול סרטני – יש מומחים המאמינים כי המחלה למעשה מקושרת להפרעות זקפה שעלולות להיגרם לאחר הניתוח
- הפרעות זקפה על רקע סוכרת – גורם המעלה את הסיכון להתפתחות מחלת פיירוני פי 4 או 5 בהשוואה לאוכלוסייה הכללית
- גיל מבוגר
- היסטוריה משפחתית של מחלת פיירוני – במשפחות בהן קרובים בדרגה ראשונה (אב או אח) חלו בפיירוני הסיכויים לחלות עולים משמעותית
הטיפול במחלת פיירוני
אמצעי הטיפול השונים מותאמים לשלב המחלה: בשלב הפעיל הטיפול יתמקד בניסיון להאט את התקדמות המחלה והפחתת הכאב. בשלב הכרוני הטיפול יתמקד בניסיון ליישר את עקמומיות הפין ככל שניתן ובשחזור יכולת התפקוד המיני, במידה והיא נפגעה.
במקרים בהם נגעי הפלאק קטנים, אין עקמומיות בפין או שהיא מועטה, אין כאבים, אין בעיות בקיום יחסי מין ובהשתנה – יתכן ולא יידרש כל טיפול. במידה ונחוץ טיפול, האורולוג המטפל יחליט האם צריך טיפול ניתוחי או לא – תלוי בחומרת הסימפטומים ובשלב המחלה.
1. טיפולים שאינם ניתוחיים מתאימים לשלב הפעיל והם מבוססים על נטילת תרופות בכדורים (הפועלים במנגנונים נוגדי דלקת שונים) או הזרקת החומר הפעיל ישירות לתוך הרקמה המצטלקת.
- הזרקות מתבססות על:
- קולגנאז – זהו אנזים שמסייע לפרק את הפלאק, מה שתורם להפחתת עקמומיות הפין ומשפר את הזקפה. זהו טיפול שעשוי לייתר את הצורך בניתוח
- תרופה להורדת לחץ דם – עשויה לסייע להפחית את הכאב ואת העקמומיות בהזרקה לתוך הפלאק
- אינטרפרון אלפא 2b – אינטרפרון הוא חלבון הנוצר על ידי תאי מערכת החיסון. מחקרים הראו כי הוא מפחית כאב, את עקמומיות הפין ואת גודל הפלאק
- תרופות – נכון לעכשיו אין טיפול תרופתי המשפיע ביעילות על עקמומיות הפין. קיים טיפול תרופתי (הניתן גם עבור כוויצת דופויטרן) שעשוי להפחית את גודל נגעי הפלאק. תרופות נוגדות דלקת ממשפחת ה- NSAIDs ניתנות לשיכוך כאב.
מלבד קולאגנאז, שאינו זמין באירופה, כל יתר ההזרקות או התרופות לא הוכחו כגורמים לשיפור משמעותי
- סוגי טיפולים נוספים שעדיין נחקרים כוללים:
- מכשירי ואקום ומכשירי משיכה מכנית – למתיחת הפין והפחתת העקמומיות
- טיפול בגלי הלם – המתמקדים בריסוק ההסתיידויות והפחתת כאב
- טיפול עם גלי רדיו (ורטיקה) – שיקום של רקמת הטוניקה באמצעות חידוש סיבי קולגן. כמו בשיקום הרקמות בהפרעות זקפה, ההנחה היא שבאמצעות טיפול טבעי ניתן יהיה גם לסייע בהתמודדות עם עקמת הפין.
2. מיעוט החולים להם נגרם עיוות של הפין או הפרעה משמעותית בתפקוד המיני יזדקקו לטיפול ניתוחי כדי ליישר את האיבר, לשמר את אורכו ואת התפקוד הזקפתי. אחוזי ההצלחה של הניתוחים נחשבים לגבוהים מאוד:
- כשאין ברקע הפרעות זקפה – יבוצעו ניתוחים שמטרתם ליישר את הפין על ידי קיצור הצד הארוך. אפשרות ניתוחית אחרת היא הסרת הפלאק והשתלת רקמה בריאה במקומו שתוסר מאזור אחר בגוף או תילקח מחומר סינטטי, כדי לשחזר חלק מהאורך המקורי של הפין.
- כשיש ברקע הפרעות זקפה – יישקל ניתוח השתלת תותב בפין. יש מקרים בהם השתלת התותב תגרום בפני עצמה ליישור הפין. במידה ולא, ישולבו בנוסף אחד משני הניתוחים הנ”ל ליישור הפין.
החברה מבהירה בזאת כי המידע הכלול באתר הינו למטרות מידע בלבד, ואינו נועד להוות תחליף לייעוץ רפואי ובריאותי מקצועי ואינו מהווה ייעוץ או חוות דעת רפואית. פנה תמיד לייעוץ אצל הרופא שלך או גורם מוסמך אחר בכל מצב רפואי או שאלה שיש לך לגבי מצבך הרפואי.